
Last night, I was wistful for a very long moment for the pre-pandemic, pre-COVID-19 world, as I spotted the Hub restaurant and the Strand Theatre straight ahead of me downtown on Churchill Drive here in Thompson, Manitoba. After almost a year of takeout cuisine, which I am indeed grateful for, the Hub’s dining room, and perhaps a very rare steak sandwich to enjoy in the company of friends, and/or a movie next-door at the Strand Theatre, reminded me of life before Code Red.
For the last year, I have like many, many other people around the world, focused primarily on the present and putting one foot in front of the other and moving forward, one day at a time. It can be exhausting. Last March, the calendar may have said 31 days, but in truth it was the month without end.
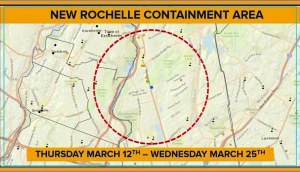
One of the most chilling things, and there have been many, that I’ve heard to date during the COVID-19 pandemic, was this audio clip posted on Twitter last March 21. I heard this brief 30-second clip on Twitter March 24, 2020, the day after the “surge” hit New York City. Tim Mak is National Public Radio (NPR’s) Washington investigative correspondent – and an emergency medical technician (EMT), which is how he got the message. Aside from the subject matter, there is something eerie about that electronically-generated voice on the automated message that went out, with this message:
“This an emergency message. This is a priority request for D.C. MRC volunteers (District of Columbia (DC) Medical Reserve Corps (DC MRC)…” (https://twitter.com/i/status/1241471610395267084)
The District of Columbia (DC) Medical Reserve Corps (DC MRC) supports the DC Department of Health (DC Health) in its role as lead for public health and medical emergency preparedness, response and recovery by recruiting, training, and deploying medical and non-medical volunteers to assist with planned events and emergencies.
On March 30, I wrote on Facebook: “Consider this. Ordered earlier this month to “lean forward,” a military term familiar to those who serve in the United States Navy, meaning the willingness to be aggressive, to take risks, the U.S.Navy hospital ship USNS Comfort (T-AH-20), homeported at Naval Station Norfolk, Virginia, sailed from port up the Atlantic seaboard Saturday and arrived in New York Harbor this morning.
“The Comfort will provide relief for New York hospitals by taking on non-COVID-19 cases and allowing the hospitals to focus on the most critical patients suffering from the virus.
“Picture this.
“What those sailors, military doctors and nurses, officers, enlisted personnel and civilians aboard the USNS Comfort (T-AH-20) must have been thinking as they answered the call of duty and sailed north into a Biological Armageddon.”
The following day, on March 31, 2020, I posted again on Facebook, “Waking up every morning in March 2020: ‘Red alert. All hands stand to battle stations'” (https://www.youtube.com/watch?v=wV30YwXaKJg).
I’ve read, thought and written a fair bit about pandemics and the like over the last 30 years. More than a decade ago on Dec. 4, 2010, when I was editing the Thompson Citizen and Nickel Belt News, I penned a story headlined, “Potential influenza pandemic on Garden Hill First Nation, MKO says: Surrounding Island Lake First Nations may also be under the flu gun.”
I wrote: “The novel H1N1 influenza pandemic, which started in Mexico in March 2009, albeit with relatively mild symptoms in most cases, was the first pandemic since the Hong Kong Flu of 1968. It originated in Guangdong Province in southeast China, but the first record of the outbreak was in Hong Kong on July 13, 1968.
“By the end of July, extensive outbreaks were reported in Vietnam and Singapore. By September 1968, Hong Kong Flu reached India, Philippines, northern Australia and Europe. That same month, the virus entered California via returning Vietnam War troops but did not become widespread in the North American until December 1968.
“A vaccine became available in 1969 one month after the Hong Kong flu pandemic peaked in North America. About a million people died worldwide in what are described as “excess” death beyond what be expected in a normal flu season, but still only half the mortality rate of the Asian flu a decade earlier. H1N1 swine flu is the first worldwide influenza pandemic since the Hong Flu of 1968-69.
“A decade earlier, the Asian Flu pandemic of 1957 was an outbreak of avian-origin H2N2 influenza that originated in China in early 1956 and lasted until 1958. It originated from mutation in wild ducks combining with a pre-existing human strain. The virus was first identified in Guizhou and spread to Singapore in February 1957, reaching Hong Kong by April and the United States and Canada by June 1957. Estimates of worldwide deaths caused by the Asian Flu pandemic vary, but the World Health Organization believes it is about two million.
“The Asian Flu strain later mutated through antigenic drift into H3N2, resulting in the milder Hong Kong Flu pandemic of 1968 and 1969.
“Influenza A viruses are classified into subtypes on the basis of two surface proteins: hemagglutinin (H) and neuraminidase (N).
“Three subtypes of hemagglutinin (H1, H2 and H3) and two subtypes of neuraminidase (N1 and N2) are recognized among influenza A viruses that have caused widespread human disease, says the Public Health Agency of Canada. “Since 1977 the human H3N2 and human H1N1 influenza A subtypes have contributed to influenza illness to varying degrees each year. It is not yet known if this pattern will be altered by the emergence of the 2009 pandemic virus [A/California/7/2009 (H1N1)]. Immunity to the H and N antigens reduces the likelihood of infection and lessens the severity of disease if infection occurs.”
“Influenza B viruses have evolved into two antigenically distinct lineages since the mid-1980s, represented by B/Yamagata/16/88-like and B/Victoria/2/87-like viruses. Viruses of the B/Yamagata lineage accounted for the majority of isolates in most countries between 1990 and 2001. Viruses belonging to the B/Victoria lineage were not identified outside of Asia between 1991 and 2001, but in March 2001 they re-emerged for the first time in a decade in North America. Since then, viruses from both the B/Yamagata and B/Victoria lineages have variously contributed to influenza illness each year.
“The antigenic characteristics of current and emerging influenza virus strains include A/California/7/2009 (H1N1)-like, A/Perth/16/2009 (H3N2)-like and B/Brisbane/60/2008 (Victoria lineage)-like antigens.”
On Nov. 1, 2019, just before a likely, but not yet conclusively proven, viral species jump to humans, in or around Wuhan, China, that likely sparked the severe acute respiratory syndrome coronavirus SARS-CoV-2, more commonly known as COVID-19, I posted on Facebook on time-lapse tracking of the transmission and evolution of Influenza A (H7N9), the most deadly flu on Earth, which has been circulating in China for the last five years or so. It has a mortality rate of 40 per cent, making it about 200 times more deadly than 2018’s Influenza A (H3N2) flu virus that circulated in Canada.
While influenza isn’t a coronavirus, some of the arguments I made on Oct. 16, 2013 in a editorial for the Thompson Citizen, might sound somewhat familiar today, “Even if the influenza vaccine only prevents infection 60 per cent to 70 per cent of the time, in the best of cases – meaning that of every 10 people who would have gotten the flu without the shot, three or four still will – flu shots have proven to be effective in slowing the virus down and helping to limit the spread of pandemics,” I wrote. “On the balance of probabilities, you hopefully are helping yourself in getting a flu shot, but you’re almost certainly in any event being altruistic in helping the rest of us in the general population by slowing the spread the virus down.”
I’ve also blogged in soundingsjohnbarker on such esoteric topics as blog posts on “Black Death: Not so bad?” in 2014, “What if the 22nd century means staying at home with long-distance travel a thing of the past?” in 2015, “A still bigger picture: Médecins Sans Frontières’ (MSF), Samaritan’s Purse, ZMapp and the 2014 Ebola Crisis” in 2018 and, more recently, “The fire this time? Pandemic prose, and waiting and watching for the ‘big one’” in 2020
Thirty years ago, I wrote a third-year history essay at Trent way back in 1991 about ergot poisoning, from a fungus that commonly forms in wheat, rye, and other grains, and is now known to cause such symptoms as convulsions, vomiting, and hallucinations, possibly triggering the events leading to the Salem witch trials in Massachusetts between February 1692 and May 1693. In 2006. I read Laurie Garrett’s landmark 1994 book, “The Coming Plague: Newly Emerging Diseases in a World Out of Balance.”
In 2011, Megan O’Brien was able to tell me she could bring in on inter-library loan to the Thompson Public Library for me a copy of “The Great Mortality: An Intimate History of the Black Death, the Most Devastating Plague Of All Time” by John Kelly, published in 2005.
Four years later, I borrowed an audio book version from University College of the North’s Wellington & Madeleine Spence Memorial Library on the Thompson Campus of “Station Eleven”, New York City writer Emily St. John Mandel’s post-apocalyptic novel published in 2014, and centred around the fictional “Georgia Flu” pandemic, which is so lethal, and named after the former Soviet republic, that within weeks, most of the world’s population has been killed and “all countries and borders have vanished.”
In 2017, also from the UCN library here, I borrowed “The Plague”, a novel by Albert Camus, published in 1947, that tells the story from the point of view of an unknown narrator of a plague sweeping the French Algerian city of Oran.
I spent Mondays between 5 p.m. and 6 p.m. in a comfortable orange chair on the third floor of UCN during the fall of 2019 reading John M. Barry’s book “The Great Influenza: The Story of the Deadliest Pandemic in History”, chronicling the 1918-19 Spanish Flu pandemic. Barry is an adjunct member of faculty at the Tulane University School of Public Health and Tropical Medicine in New Orleans.
So, yes, I had some idea of what a pandemic might look like when it arrived a year ago and it did turn out indeed to be the fire this time.
Knowing might be good preparation. But you can only know so much. Nowhere had I read in advance to get ready for a pandemic where perhaps one out of every three carriers might be showing no symptoms and feeling just fine while shedding the virus and transmitting a disease, with multiple variants now, and that varies so much in its effects from person to person. The Chimera, according to Greek mythology, was a monstrous fire-breathing hybrid creature. COVID-19 is its progeny.
And no matter how much you know, it’s not the same as the lived experience of a pandemic where “mask up” is the imperative public health-ordered emergency non-pharmaceutical intervention that taken to brain and heart, along with six-foot physical so-called “social distancing” and restricted travel, might just some day mean dinner at the Hub and a movie at the Strand Theatre again.
That might seem like a distant hope at the moment, and I suppose it is, but I am mindful that individual actions can collectively matter, and instead of the “twindemic” of influenza and COVID-19 public health epidemiologists feared last spring for this winter, the start of the annual flu season in the Northern Hemisphere has been very quiet to date, much like it was in the Southern Hemisphere during their winter season last year during our summer. Since September, the CDC “FluView” – its weekly report on influenza surveillance – has shown all 50 states in shades of green and chartreuse, indicating “minimal” or “low” flu activity. Normally by December, at least some states are painted in oranges and reds for “moderate” and “high.”
In the Southern Hemisphere, where winter stretches from June through August, widespread mask-wearing, rigorous lockdowns and other precautions against Covid-19 transmission drove the flu down to record-low levels. Southern Hemisphere countries help “reseed” influenza viruses in the Northern Hemisphere each year, so a good flu season here year “Down Under” often, not always, means we can reasonably hope for one in the Northern Hemisphere.
And some of it is just seasonal variability. Some flu seasons are worse than others. Flu viruses mutate far more than coronaviruses through antigenic drift, hence the need for a different combination flu vaccine every year.
Since last February, COVID-19 has killed more than 430,000 people in the United States, more than influenza has in the last five years, notes the Johns Hopkins Bloomberg School of Public Health.in Baltimore. COVID-19 has a higher severe disease and mortality rate than influenza in all age groups, except perhaps children under the age of 12. “Influenza is a significant burden on the population, but COVID-19 has had a vastly larger effect,” Johns Hopkins says.
You can also follow me on Twitter at: https://twitter.com/jwbarker22
55.736962
-97.864877


 While some 675,000 Americans died over three years between January 1918 and December 1920 during the three waves of the Spanish Flu pandemic, the country’s population was 103.2 million. Today, the population of the United States is more than 331 million. The world population in 1918 was about 1.8 billion, compared to about 7.8 billion people today.
While some 675,000 Americans died over three years between January 1918 and December 1920 during the three waves of the Spanish Flu pandemic, the country’s population was 103.2 million. Today, the population of the United States is more than 331 million. The world population in 1918 was about 1.8 billion, compared to about 7.8 billion people today.
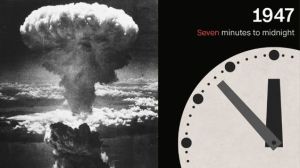
 The rolling real time daily death count on the online COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) in Baltimore functions as our equivalent of the Bulletin of the Atomic Scientists’ “Doomsday Clock,” circa 1947, and the clock itself, set at 100 seconds before midnight last Jan. 27, is being profoundly influenced by COVID-19.
The rolling real time daily death count on the online COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) in Baltimore functions as our equivalent of the Bulletin of the Atomic Scientists’ “Doomsday Clock,” circa 1947, and the clock itself, set at 100 seconds before midnight last Jan. 27, is being profoundly influenced by COVID-19.